Bad Weather Brings Flu – Makes Sense
By Shlomo Maital
The conflation of COVID-19 and the fall/winter influenza season worries public health officials. In Israel, hospitals are already over-stretched – and doctors and nurses dread the onslaught of flu patients, on top of several thousand new COVID-19 cases daily. This is why Israel is now in partial lockdown, during the High Holydays.
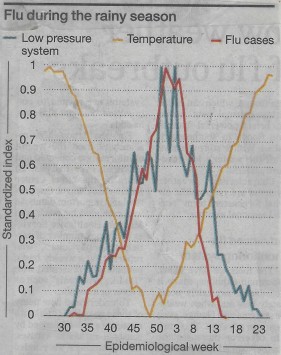
A new study by a group of Israeli and Mideast scholars shows, for the Eastern Mediterranean, a close correlation between climate and flu. *
The orange line above shows temperature. The red line: % of the population with flu. And the blue line: barometric pressure (inverted – high scale means low pressure). All three variables have been converted to a standardized zero to one normalized scale.
So – what is the connection between weather and flu?
It is pretty simple. Flu spreads through contact from one person to another. Outdoors, winds, even light breezes, disperse flu particles from sneezes and coughs and breathing. Indoors, this is far less true. In bad weather, people spend more time indoors. Hence, more flu.
This finding seems relevant for COVID-19 too. A friend of mine, a veteran pulmonary medical specialist, observes:
“With each cough and sneeze, there are very small particles under 10 microns in diameter, especially those under 2.5 microns, that tend to remain suspended in the air for a long time. This aerosol is scattered all over. While the volume of these particles is low, their surface area is large and lots of virus particles can stick to the surface of these small particles. It is now fully accepted that the virus’ transmission by aerosols is an important vector. The relatively large area of the eyes’ surface makes them vulnerable to the landing and culture of viruses. Protection against sprays and eye protection are crucial to creating barriers against contracting COVID-19.”
“Cough is the dominant mode of spread and as such should be monitored in areas where people congregate to assess risk in an objective mode and to identify possible spreaders. Cough monitoring is feasible with devices being available and used in pulmonary and occupational contexts.”
“The dilution in open air is immense. Consider the following example: A soft wind is blowing at 3.6 km/hour (2.2 miles per hour). If we consider a 4-meter- long test volume of air, the flow of air in the wind will sweep the test volume in four seconds, or nearly a thousand times per hour. This is significant and should be sufficient to prevent infection if very sporadic individuals are present. But if a distance of two meters cannot be observed at all times, the risk level is such that the use of a mask, at least surgical or cloth, is still required in the open.”
So, the message here is clear. We MUST get this second wave of COVID-19 under control before the flu season. If we don’t we will have two problems:
- Bad weather will bring influenza, and some flu sufferers will need hospitalization
- Bad weather will send people indoors, and COVID-19 spreads more easily there.
Hochman, A., Alpert, P., Negev, M., Abdeen, Z., Abdeen, A. M., Pinto, J. G., & Levine, H. (2020). The relationship between cyclonic weather regimes and seasonal influenza over the Eastern Mediterranean. Science of The Total Environment, 141686.


Leave a comment
Comments feed for this article